Becoming a new parent is often portrayed as a joyous time, but the reality can be far more complex. The postpartum period brings significant changes, physical challenges and sleep deprivation that can greatly affect a parent’s emotional well-being.
Many new parents experience temporary “baby blues,” but for some, these feelings develop into postpartum depression or anxiety. In fact, up to 15% of new parents will go on to develop postpartum depression, indicating a deeper, more persistent mental health challenge. It can be difficult to distinguish between normal new-parent worries and more serious mental health concerns.
Both birth and non-birth parents can struggle with these issues, which may stem from various factors including birth complications, hormonal changes, or feeling overwhelmed by new responsibilities. These challenges can strain relationships and be particularly daunting for single parents.
Today, we’ll explore postpartum depression in detail, helping parents recognise the difference between typical postpartum emotions and postpartum depression. We’ll also share how to seek support, emphasising that getting help early can lead to better results for you and your family.
Postpartum depression symptoms
You are likely to hear lots of labels for perinatal depression as an expecting or new parent, including perinatal depression or anxiety, postnatal depression, postpartum depression or even the ‘baby blues’. ‘Perinatal’ includes the whole of the pregnancy and up to when your baby is one year old, so perinatal depression is referring to this timeframe.
Postpartum is a medical term for the period 6 weeks after birth. When it comes to depression, postnatal or postpartum means the time up to 12 months after giving birth. We are using the 12 month timeframe definition for this blog and using the terms postnatal and postpartum interchangeably.
Postpartum or postnatal anxiety is referring to the same 12 month timeframe, but where symptoms present more like fear, worry or panic than depressive symptoms, which are more likely to include sadness, hopelessness and feeling unworthy.
Experiencing symptoms of postnatal depression or anxiety are more common than you might think, with 1 in 5 mothers or birth parents affected and 1 in 10 fathers or non birth parents affected. We often explain this to parents to reassure them that these symptoms are valid, happen frequently and can reflect how difficult this time can be.
We recognise at ForWhen that postnatal depression doesn’t necessarily fit into neat timeframes, which is why we are available for support from conception up until the first year for your baby.
Early Symptoms of postpartum depression
The first few weeks post birth are likely to be emotional for most women, with the physical effects and hormonal changes of giving birth combined with the stress of caring for a new-born often resulting in symptoms similar to those of postpartum depression. These symptoms can include mood swings, which are part of the emotional upheaval that arises after childbirth.
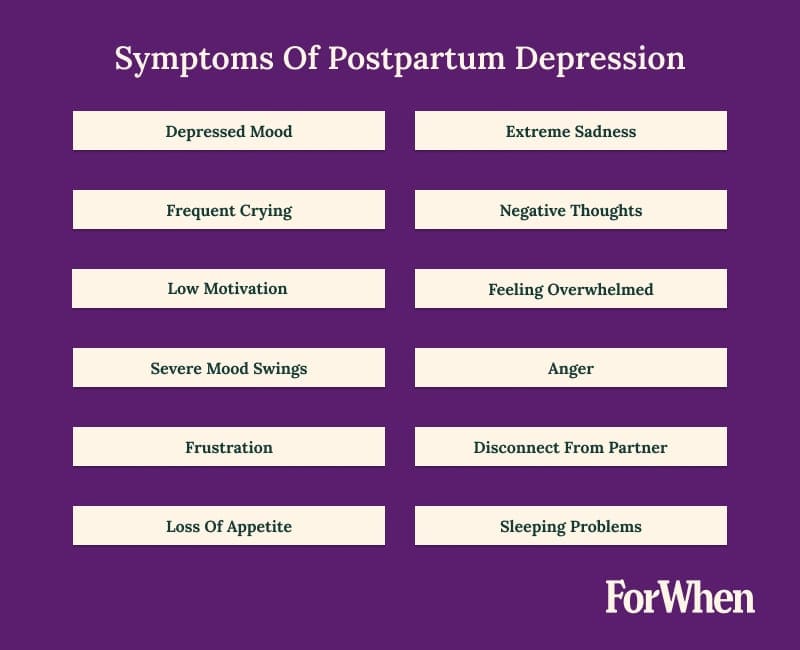
Look out for the following symptoms: low mood, extreme sadness, frequent crying spells or excessive crying, or being unable to sleep when your baby is sleeping. You may also experience negative thoughts, loss of interest in activities you previously enjoyed, feeling as though nothing can cheer you up, lacking hope for the future and feeling completely overwhelmed by everyday tasks.
While some emotional challenges are normal with a new baby, persistent symptoms that disrupt daily life may indicate a need for support. Excessive worry, constant anxiety, or panic attacks could also signal postpartum depression or anxiety, which often occur at the same time.
Panic attacks can be frightening and may be mistaken for heart attacks due to symptoms like chest pain, shortness of breath, and a racing heart. Those with a history of antenatal depression or anxiety should look out for potential symptoms in the postnatal period.
Recognising postpartum depression can be challenging. If you’re unsure, it’s best to seek support early – your emotional health is crucial. Early intervention leads to better outcomes for you and your family.
Treatment options for postnatal depression vary, and it’s important to remember that you’re not alone. Seeking support is a brave step forward. Professional help, including talking with your GP/healthcare provider is a good place to start, even if you’re not ready to discuss your feelings with friends or family.
Key Highlight
There are various ways to treat depression in the postnatal period and treatment options should never be ‘one size fits all’. Some people feel uncertain about what a postnatal depression diagnosis may mean or be worried about admitting they aren’t coping.
Recognising Postnatal Depression (PND) vs Baby Blues Symptoms
Baby blues
You may have heard the term ‘baby blues’ and may (like me) feel it doesn’t quite cut it to describe the level of emotions experienced after giving birth. Baby blues refers to the 3-5 days after giving birth when the birthing parent can experience a whole range of emotions that last up to a week. So when do the baby blues become postnatal depression and what can you do about this?
Postnatal depression
Postpartum or postnatal depression may be diagnosed by a Psychologist, a Psychiatrist, or your GP and is longer lasting, with more severe symptoms than baby blues. The Edinburgh Postnatal Depression Scale is often used to help identify when PND may be occurring. It is likely that when there is severe postnatal depression or additional mental illness, you may need more specialised support.
Severe PND
We want to acknowledge firstly that both being a new parent or experiencing a mental health condition can be incredibly difficult experiences and the combination of these can result in more complex issues. These next paragraphs talk about suicide and suicidal thoughts, so please be aware before reading on.
So what are signs of severe postpartum depression?
These symptoms may still be sadness, anger, hopelessness and despair but are likely to be more frequently occurring and longer lasting than in milder cases of postnatal depression. They will have more impact on your day-to-day life. In severe cases these symptoms are likely to cause feelings of wanting to give up, run away or even contemplate self-harm, harming others, death or suicide as a way to escape. It is likely in severe cases that screening tool scores, like the Edinburgh Postnatal Depression Scale, will be higher.
Even for severe postnatal depression there are treatments which are effective and can help.
Postpartum psychosis
There is a low risk in the postpartum period for birth parents to experience psychosis, regardless of whether there is a history of this, although the risk is higher with previously diagnosed mental illness.
Postpartum psychosis, also known as puerperal psychosis, is less common than postnatal depression, impacting 1-2 in 1000 birth parents. It is defined as occurring within days to one month following birth. It includes unusual thoughts and beliefs like someone is trying to harm the baby, finding it hard to sleep, feeling full of energy or restless and irritable or feeling invincible. Due to this, it is critical to recognise and manage symptoms for postpartum psychosis and get urgent assistance.
Risk factors for Postpartum Depression
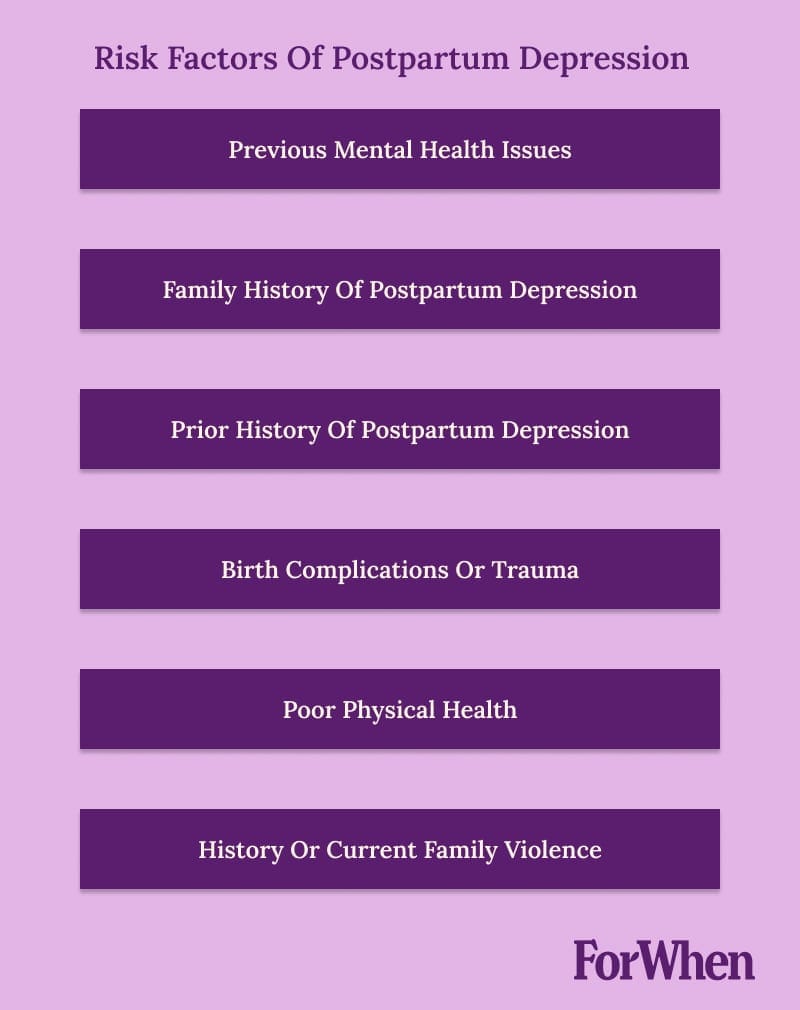
Increased risk means higher level or more risk factors are present, which may contribute to the likelihood or severity of postnatal depression. It is important to know that while risk factors can contribute to postpartum depression, the presence of these does not automatically mean that you will develop postnatal depression.
A woman’s risk for experiencing postpartum depression is increased with a history of mental health issues. If you have experienced anxiety or depression in the past, there is a higher risk of developing postnatal depression. Previous diagnoses of Bipolar Disorder, Postpartum Depression or Postpartum psychosis are especially important to consider.
While somewhat limited information exists for perinatal bipolar disorder, an existing diagnosis is more likely to result in a relapse of symptoms during pregnancy and untreated, can cause complications for pregnancy and birth. It is especially important for this reason that symptoms are managed throughout pregnancy, to promote positive outcomes for both parents and the baby.
If you have a family history of mental health issues, this can be a risk factor for postnatal depression. This includes bipolar disorder and postpartum depression.
Pregnancy or birth complications are also important factors to consider. This could include concerns about the development of the unborn child or medical issues for the mother or baby during pregnancy or at the time of birth.
Poor physical health of parents is a risk factor for poor emotional health. It is important to find time to prioritise this, with the support of any healthcare professionals, friends and family.
Stressful events in your environment, such as a history of trauma or the presence of family violence, are also risk factors for postnatal depression. Less obvious stressful events might include big life transitions, like changing jobs, financial changes or renovating your house.
The good thing about understanding risk factors for postnatal depression is that you have control over some of these – not all, but some! Which means you have the ability to put supports in place, which may result in improved outcomes for your family.
Postpartum Depression in Fathers & Non-Birth Parents
While often overlooked, up to 10% of fathers and non-birth parents experience postpartum depression (PPD). This under recognition can lead to delayed diagnosis and treatment.
Symptoms in non-birth parents may differ from those typically seen in birth mothers:
- Increased irritability or anger, such as outbursts or constant frustration
- Feeling disconnected from family or emotionally numb towards the baby
- Doing risky behaviours, such as an increase in substance use or reckless driving
- Working excessively as a form of escape from home life
- Experiencing physical symptoms like ongoing headaches, gut issues, or changes in appetite
- Difficulty concentrating or making decisions, even on simple tasks
- Feelings of worthlessness or feeling trapped by new responsibilities
Risk factors specific to non-birth parents include:
- History of depression or other mental health issues
- Relationship stress or feeling excluded from the mother-baby bond
- Financial pressures, especially if they’re now the only breadwinner
- Sleep deprivation, which can be severe in the early months of parenting
- Feeling unprepared for parenthood or overwhelmed by new responsibilities
- Lack of support systems
- Hormonal changes, which can also occur in fathers during the postnatal period
The impact of PPD on non-birthing parents can be significant, affecting bonding with the baby, relationship with partners and overall family dynamics. It’s crucial to recognise that PPD can affect any parent, regardless of gender or biological relation to the child.
Early recognition of these unique symptoms and risk factors is key to ensuring all parents receive the support and treatment they need during the transition to parenthood.
Managing The Symptoms of Postpartum Depression
Self care is important when managing symptoms of postnatal depression &/or anxiety. Some ideas for self care are:
- making sure you shower
- keeping a healthy diet
- regular sleep
- doing something you enjoy
- watching your favourite TV show
- reading a book
- exercising
- spending time with family and friends
- practicing mindfulness
Prioritising yourself will ‘fill your cup’ a little each and every day to continue caring for your baby.
Mindfulness and self-care (why not use both?) can make a world of difference to coping each day as a new parent. Becoming a new parent, you may need to adjust previous thinking and learn to lean on others, whether family, friends or professionals. Asking for help can be difficult but can support you to manage the symptoms of depression by offloading some tasks or having time to rest or sleep.
Key Highlight
A couples approach to treatment, acknowledging joint experience of postpartum depression symptoms has been shown to help families better adjust to parenthood as mothers and fathers both experience postpartum depression and anxiety in different ways.
Diagnosis
Recognising symptoms assists with getting treatment. Attending your local GP for screening, assessment and possible diagnosis is a starting point. A blood test may also be suggested to assess hormone levels, as some physical health conditions cause mood fluctuation or symptoms similar to postnatal depression.
Speaking with your Child and Family Health Nurse can also provide support options including suggestions for local support groups and online resources.
Contacting a service such as ForWhen for support and guidance, may be another part of your recovery journey. This can even be before you see a GP if you’re not sure where to start.
You may be asked by any of these professionals to complete screening tools which assist with identifying postpartum depression. Professionals may also ask other questions to understand your specific circumstances and provide recommendations about the best options for you.

Treatment Options
There are a number of treatment options for postpartum depression, starting with support groups or playgroups, through to talking therapies and then if needed, antidepressant medication. Collaborating with a healthcare professional will assist to develop an effective treatment plan that’s right for you. Social workers, psychologists or counsellors can provide specialised therapeutic support in the perinatal period for parents diagnosed with postnatal depression.
A couples approach to treatment, acknowledging joint experience of postpartum depression symptoms has been shown to help families better adjust to parenthood as mothers and fathers both experience postpartum depression and anxiety in different ways.
Keeping the baby in mind when suggestions are made for treatment is an important part of promoting postnatal mental health. A newborn baby is very connected to you, so your emotional wellbeing is closely linked with that of your baby.
A GP or psychiatrist may prescribe medications such as antidepressants. They are used to stabilise low mood and reduce anxious feelings. Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressants during the postnatal period. Your GP is the best person to talk about medication with you and they will consider other factors like, whether you are breastfeeding, on other medications or are struggling with other symptoms postpartum.
Support groups
Acknowledging and asking for support is one of the key strategies to help prevent and manage postnatal depression. We know that this can seem like a really difficult thing to do, when you’re tired and busy, and feel like you should be able to manage.
Support comes in many forms – it could be from family and friends, or through more formal groups such as online, in person, community groups, and support groups or playgroups. Inclusion in these groups can provide a much-needed emotional connection to others and help you feel less alone in experiencing this hard time in becoming a new parent and experiencing postpartum depression. Think about who could be in your village.
Your Child and Family Health Nurse can suggest some support groups available in your area, there are always playgroups in each community.
If you’re not sure where to start, call ForWhen 1300 24 23 22 to talk about what’s going on and what services or supports are available in your area.

Frequently Asked Questions
See our answers below to commonly asked questions about the symptoms of postpartum depression.
The cause of postpartum depression is not fully understood. It can be attributed to many environmental, emotional, hormonal and genetic factors.
Postpartum depression is longer lasting than baby blues, symptoms are experienced for longer than 6 weeks.
Short answer is absolutely and there is support for fathers too.
Feelings of worry, tiredness and low mood can be normal when adjusting to becoming a parent it is when these symptoms continue on or get worse overtime you should seek treatment.
There is no time period when recovering from postpartum depression. It really is individual what treatment helps and how long the recovery takes.

